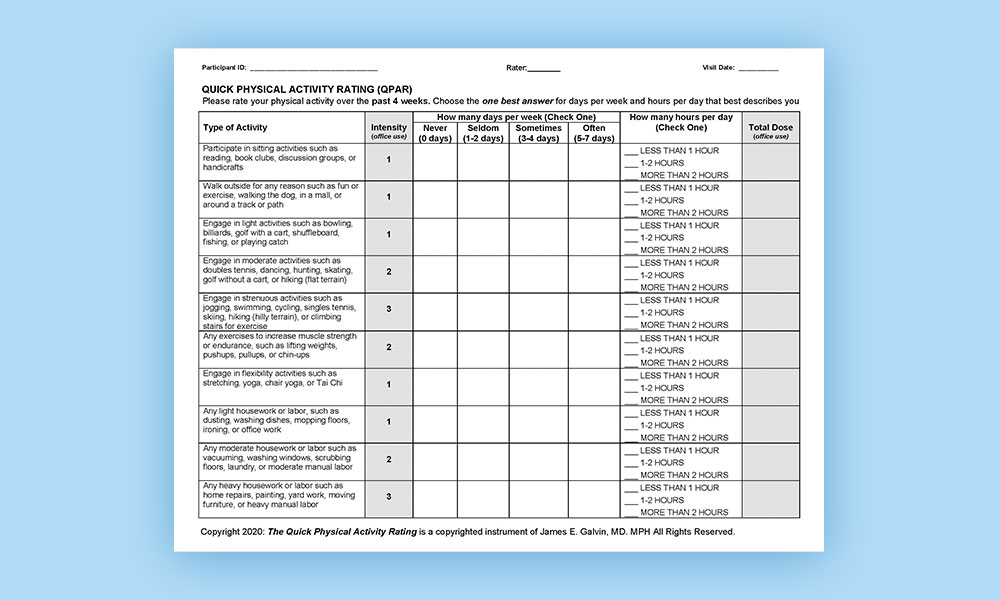
Alzheimer’s disease and related disorders (ADRD) affects over 5 million Americans and incidence is expected to increase. Over 31 million adults aged 50 and above are physically inactive and impaired physical performance may interfere with the ability to carry out activities of daily living (ADLs). Declines in physical health and activity are risk factors for ADRD and physical-cognitive impairment may have bidirectional effects on each other. It is a challenge to capture physical activity in an objective fashion. Objective measurements of physical performance and functionality can be captured during direct examination. However, direct measurement of physical activities carried on outside the clinical or research setting is not easily achieved. Our hypothesis is that a physically active individual would have higher physical performance and functionality, and less impairments in ADLs and frailty compared with an individual with little regular physical activity. Given the facts that ADRD is a significant public health problem, physical activity is an important modifiable risk factor for ADRD, physical activity is related to physical functioning – particularly in people at risk of ADRD, and the challenges of measuring physical activity facing clinicians and researchers investigating ADRD, we created a new measure, the Quick Physical Activities Rating (QPAR). The QPAR is an informant-reported instrument that quantifies the “dosage” of physical activity in healthy controls, mild cognitive impairment (MCI) and ADRD. We examined the performance of the QPAR with Gold Standard assessments of physical performance, physical functionality, and health including resting heart rate, manual dexterity, gait, mobility, strength, frailty, ADLs, health-related quality of life, and balance to establish the relationship between reported physical activity and physical functioning.
The QPAR was analyzed 390 consecutive patient-caregiver dyads who underwent a comprehensive evaluation including the Clinical Dementia Rating (CDR), mood, neuropsychological testing, caregiver ratings of patient behavior and function, and a comprehensive physical performance and gait assessment. The QPAR was completed prior to the office visit and was not considered in the clinical evaluation, physical performance assessment, staging or diagnosis of the patient. Psychometric properties including item variability and distribution, floor and ceiling effects, strength of association, known-groups performance, and internal consistency were determined. The QPAR correlated with Gold Standard assessments of strength and sarcopenia, activities of daily living, gait and mobility, fitness, health related quality of life, frailty, global physical performance, and provided good discrimination between states of physical functionality, falls risk, and frailty. The QPAR performed well in comparison to standardized scales of objective physical performance, but in a brief fashion that could facilitate its use in clinical care and research.
Like all brief tests, a positive result should be followed up with a more comprehensive evaluation or a referral to a specialist. However, in places where specialists are limited, use of the QPAR could help to more appropriately triage patients for appropriate use of services. It could also be used to follow patients in a succinct way to see how they are responding to therapy or if they have progressed and need more services. In a broader sense, a brief test such as the QPAR can be used to enroll people in research projects, and help determining prevalence of physical impairment in communities in a very quick fashion.