Number-Symbol Coding Test

Description
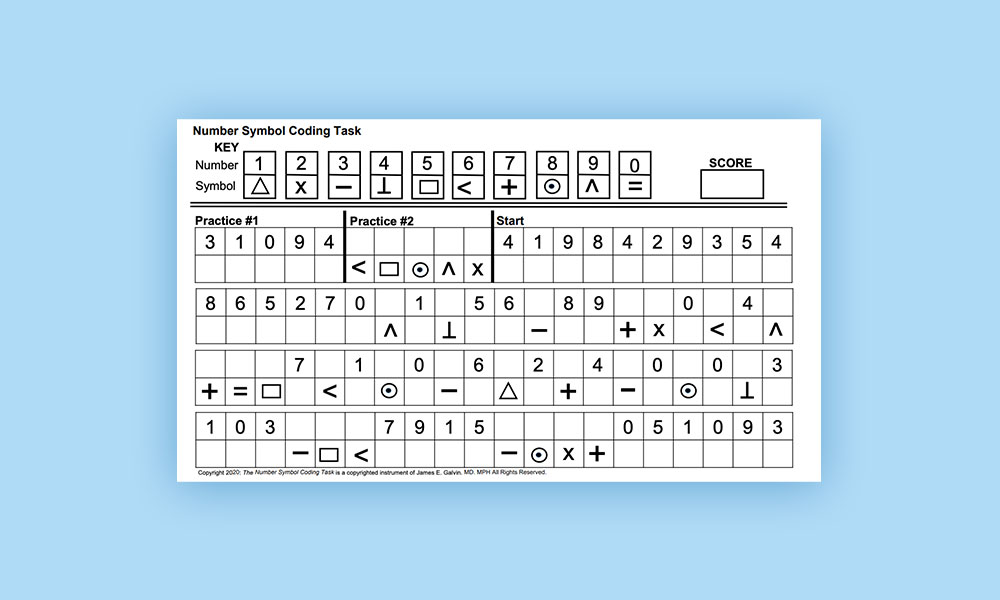
ADRD is a challenge to clinicians and researchers alike, requiring in-depth evaluations that can be time-consuming. Gold Standard evaluations such as the Clinical Dementia Rating (CDR) and comprehensive neuropsychological testing are used in many research projects but require a trained clinician to administer, interpret, and score the CDR or neuropsychological testing and require an extended period of time with the patient, and in the case of the CDR, an informant. While feasible in research settings (e.g., clinical trials, longitudinal studies), these evaluations may not be practical in primary care settings or epidemiologic caseascertainment projects [2]. Briefer evaluation tools are often used in these settings. These briefer tools can be grouped into performance-based assessments including the Montreal Cognitive Assessment (MoCA), Mini Mental State Exam, or Mini-Cog, or interview-based assessments usually with an informant such as the Quick Dementia Rating System (QDRS). These brief tests are often more heavily weighted towards capturing memory impairment, however other important domains such as attention and executive function may not be well captured. This is unfortunate because alterations in executive problem solving and decision making may be one of the earliest signs of MCI and ADRD. To address the need for a brief and easy to score test of executive function for use in clinical practice and in research, we created the Number Symbol Coding Task (NSCT).
The NSCT was analyzed 320 consecutive patient-caregiver dyads who underwent a comprehensive evaluation including the Clinical Dementia Rating (CDR), patient and caregiver versions of the Quick Dementia Rating System (QDRS), caregiver ratings of behavior and function, and neuropsychological testing, with a subset undergoing volumetric magnetic resonance imaging (MRI). Psychometric properties of the NSCT including data quality, data distribution, floor and ceiling effects, construct and known-groups validity, discriminability, and clinical profiles were determined. The NSCT followed a normal distribution. All healthy controls and MCI cases were able to complete the NSCT. The NSCT showed moderate-to-strong correlations with clinical and neuropsychological measures with the strongest association (all p’s <.001) for measures with executive components (e.g., Judgement and Problem Solving box of the CDR, Decision Making and Problem Solving domain of the QDRS, Trailmaking B, and Cognigram Attention and Executive Composite Scores). Decreasing NSCT scores corresponded to older age, worse cognitive scores, higher CDR sum of boxes scores, worse caregiver ratings of function and behavior, worse patient and informant QDRS ratings, and smaller hippocampal volumes and hippocampal occupancy scores. The NSCT provided excellent discrimination (AUC: .866; 95% CI: .82-.91) with a cut-off score of 36 providing the best combination of sensitivity (0.880) and specificity (0.759). The NSCT performed well in comparison to standardized scales of a comprehensive cognitive neurology evaluation across a wide array of sociodemographic variables in a brief fashion that could facilitate its use in clinical care and research.
Like all brief tests, a positive result should be followed up with a more comprehensive evaluation or a referral to a specialist. However in places where specialist are limited, use of the NSCT could help to more appropriately triage individuals at-risk for cognitive impairment. It could also be used to follow patients in a succinct way to see how they are responding to therapy or if they have progressed and need more services. In a broader sense, a brief test such as the NSCT can be used to enroll people in research projects, and help determining prevalence of cognitive impairment in community samples in a very quick fashion.